- Jump Around
- Individuals Interviewed
- The Healthcare Services P&L
- Revenue: New Product Offerings
- Ambient Scribing
- Risk Stratification
- Parting Thoughts
AI and the Health Services P&L
Nascent experiences in AI adoption across the Rubicon Founders portfolio
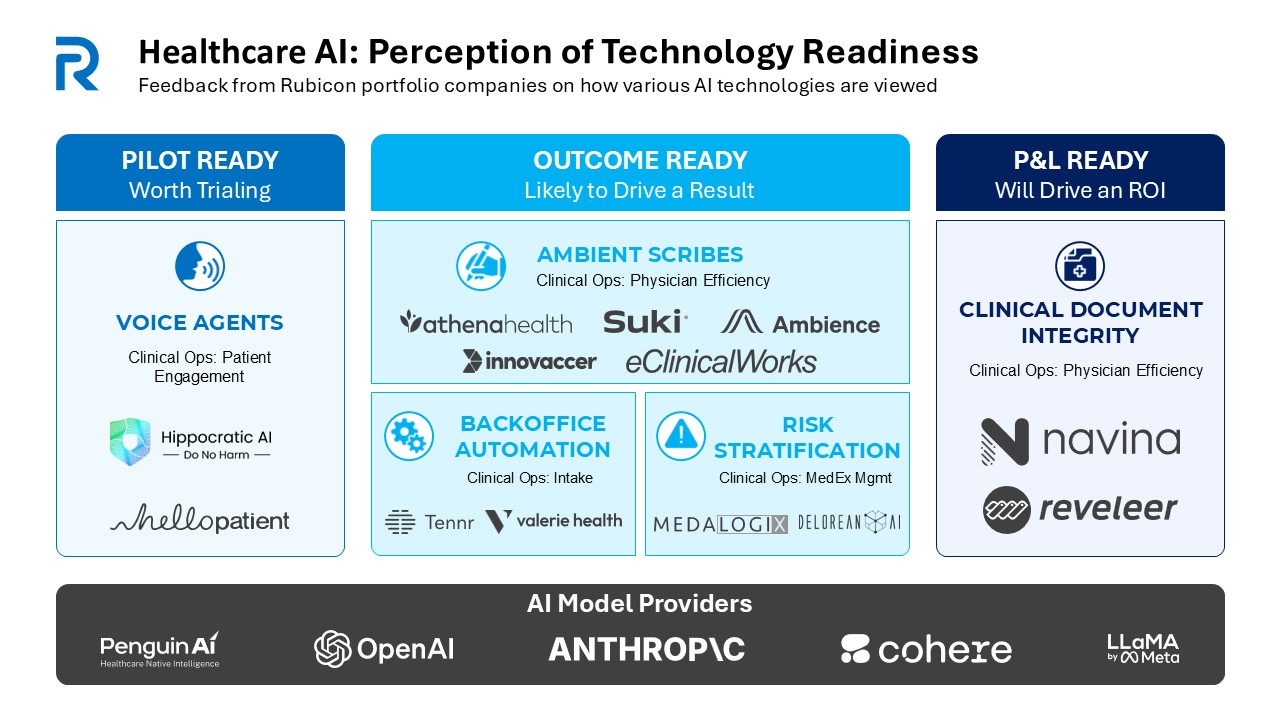
The Three Stages of AI Adoption in Healthcare
From our experience, there are three categories of AI adoption in healthcare:
- Pilot-Ready - AI tools that are technically viable but haven’t been battle-tested in real-world settings. Think of them as early-stage vaccines—promising, but not yet ready for widespread distribution.
- Outcome-Ready- These tools perform specific tasks well—summarizing patient visits, flagging missing risk codes—but they are still waiting for a measurable, hard-dollar ROI to justify their place..
- P&L-Ready - This is the gold standard: AI tools that don’t just work but pay for themselves. This is where AI stops being a science experiment and becomes an essential part of business strategy.
Where does healthcare stand. Let’s break it down.
AI Perception across the Rubicon Portfolio
The Healthcare Services P&L

Imagine a doctor’s office. Not the bustling waiting room or the buzzing nurses station, but the back office—the financial nerve center of the operation. Here, the real challenge of modern healthcare plays out. It’s not just about medicine; it’s about math.
At its core, healthcare services is a business of reliable but modest margins, where every dollar spent on human capital—nurses, technicians, administrative staff—directly impacts the bottom line. A CFO looking at the books sees not just patient care, but cost structures.
Now, introduce AI into this equation. A modest 10% reduction in clinical/service costs could drive a 41% jump in EBITDA—not because AI is taking over medicine, but because automation makes the existing system work better. AI isn’t replacing doctors. It’s helping them work faster, smarter, and more efficiently.
An Example Healthcare Services P&L
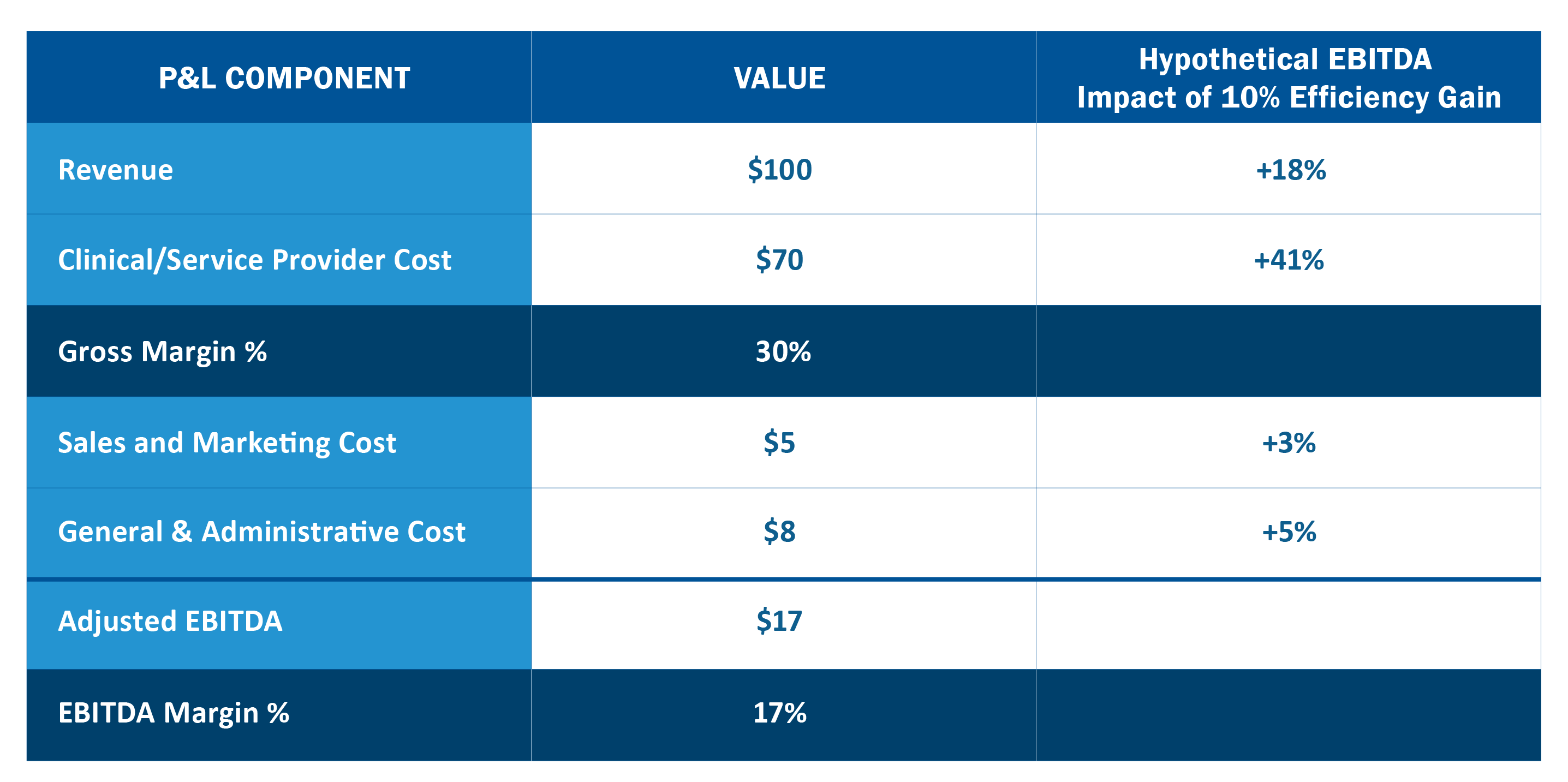
So where is AI’s potential financial impact?
- 1. The Clinical/Service Line: Small improvements in productivity have the possibility to snowball into major financial gains. Yet, despite clear economic benefits, many healthcare providers hesitate. Why? Because AI in medicine isn’t just a financial decision—it’s a cultural one. Doctors are trained to trust their instincts, not algorithms. The challenge isn’t proving AI works; it’s proving AI can be trusted.
- 2. Beyond Healthcare Costs: AI’s biggest financial win might not be in healthcare at all. Legal. Real estate. Operations. These cost centers are potentially ripe for automation, and yet, most healthcare businesses don’t think of AI in these areas. But maybe they should.
The big question isn’t whether AI can improve healthcare margins. It’s who will be savvy enough to achieve the highest ROI projects first.
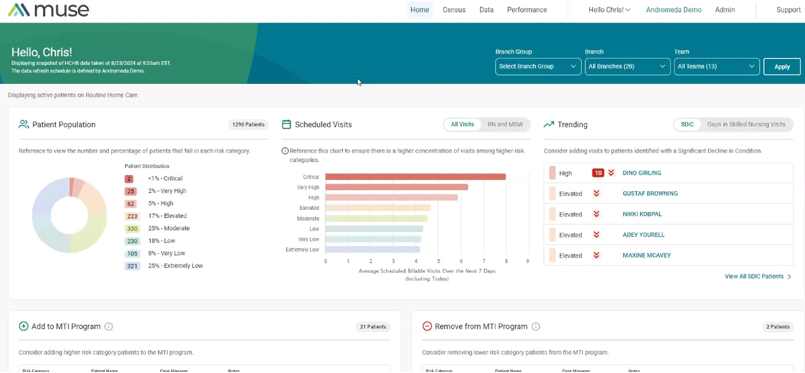
Revenue Growth and Clinical Service Management are key AI use cases in the Rubicon Portfolio
![]()
Revenue: New Product Offerings

AI offers the ability to launch new fully automated or partially automated service offerings from healthcare incumbents. We’ll explore 3 themes we’ve seen across our portfolio including: (1) Long Tail Services, (2) Volume Unlockers, and (3) Algorithmic Identifiers.
Volume Unlockers
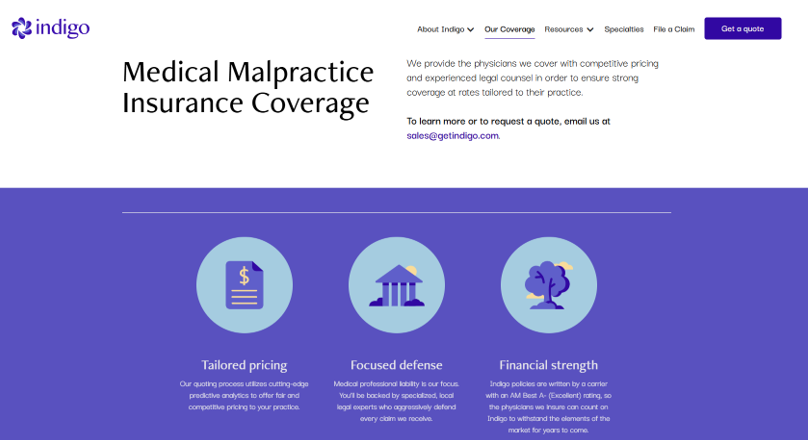
AI can help healthcare incumbents identify and service a larger range of customers. Indigo, an AI-enabled professional liability underwriter launched by Rubicon in 2022, uses a proprietary AI-enabled risk score that uses billions of data points to assess physician malpractice risk. This allows the team to avoid the worst risks and then offer a more accurate price to the target physicians in line with their actual risk profile. For lower risk doctors, this means Indigo can offer a more competitive price and win more deals. Using this proprietary model developed in-house over 2+ years, they prescored all the doctors in the U.S., which allows them to directly target the most attractive practices.
“On the back of the risk scoring model, the Indigo team will also be launching real-time quoting this year, unheard of in this space, by leveraging AI throughout the tech stack,” says Jason Foucher, the Chief Product Officer at Indigo.
The Indigo Value Prop: Using AI to better price a traditional health care service offering
Algorithmic Identifiers
Clinical service organizations are increasingly powered by unique algorithms, often focused on patient identification enabling a B2B service model by screening a third party’s patient list and matching them with services.
Cadre Hospice, a value-oriented hospice provider launched by Rubicon in 2024, is an example of this approach. Cadre applies their algorithm to a partner patient list to identify candidates for intervention, ensuring those in need of care are not overlooked and adding speed and fidelity to the process.
“In an era where payors struggle with member engagement, ensuring appropriate end-of-life care remains a critical challenge. The Cadre algorithm serves as a vital safety net, using sophisticated analytics to identify patients at the optimal time for palliative or hospice services - before they fall through the cracks in our healthcare system,” says Sonnie Linebarger, CEO of Cadre Hospice.
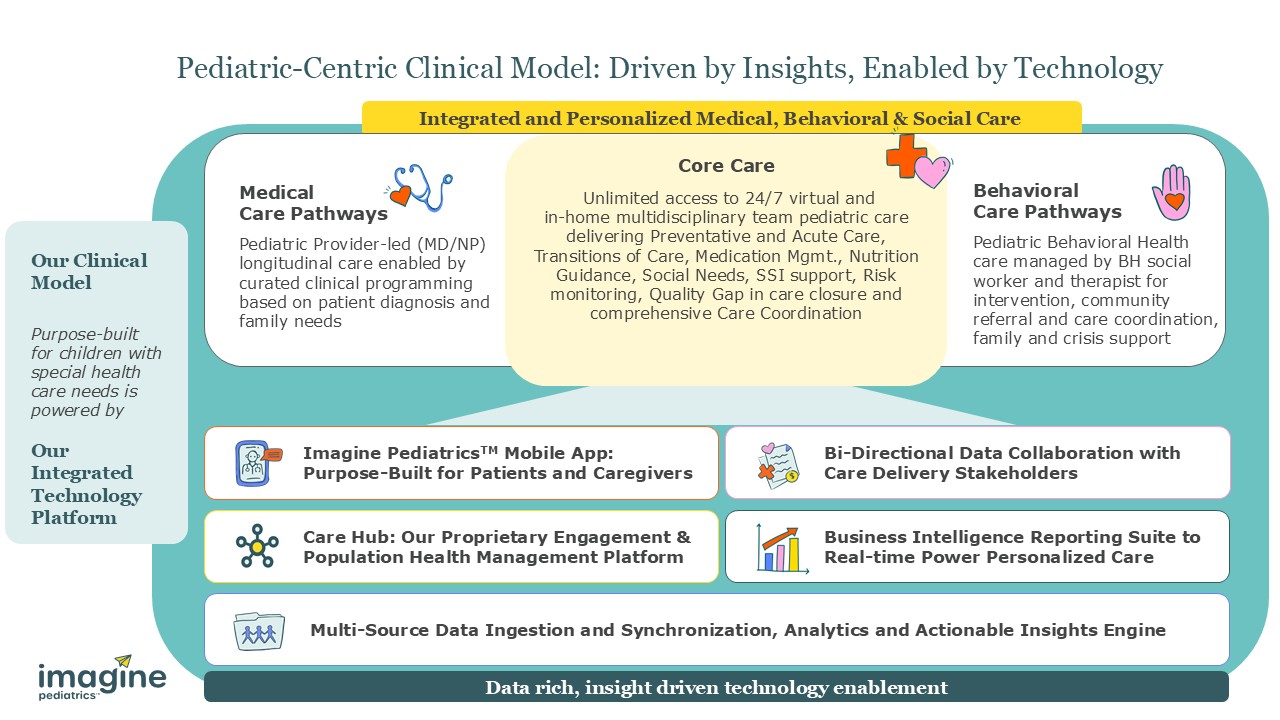
Imagine Pediatrics, launched by Rubicon in 2023, also uses an algorithmic model to identify target patients for their fully integrated, multidisciplinary, value-based pediatric care offering for children with special health care needs. In these businesses, the algorithm is woven into the care delivery model.
Like many early adopters, Imagine noted that building trust with users can be a challenge, especially if the algorithm in question is a black-box machine learning model. In those cases, similarly situated clients should consider porting the algorithm into their environment to validate it with their own data and share transparent proof points with clinical leaders.
“Value-based care arrangements require a population selection algorithm that resonates and provides your partners with ease of implementation, shows durability of clinical acuity and patient spend patterns, and avoids regression to the mean dynamics,” says Meghan Haycraft, Co-Founder and Chief Strategy Officer at Imagine Pediatrics.
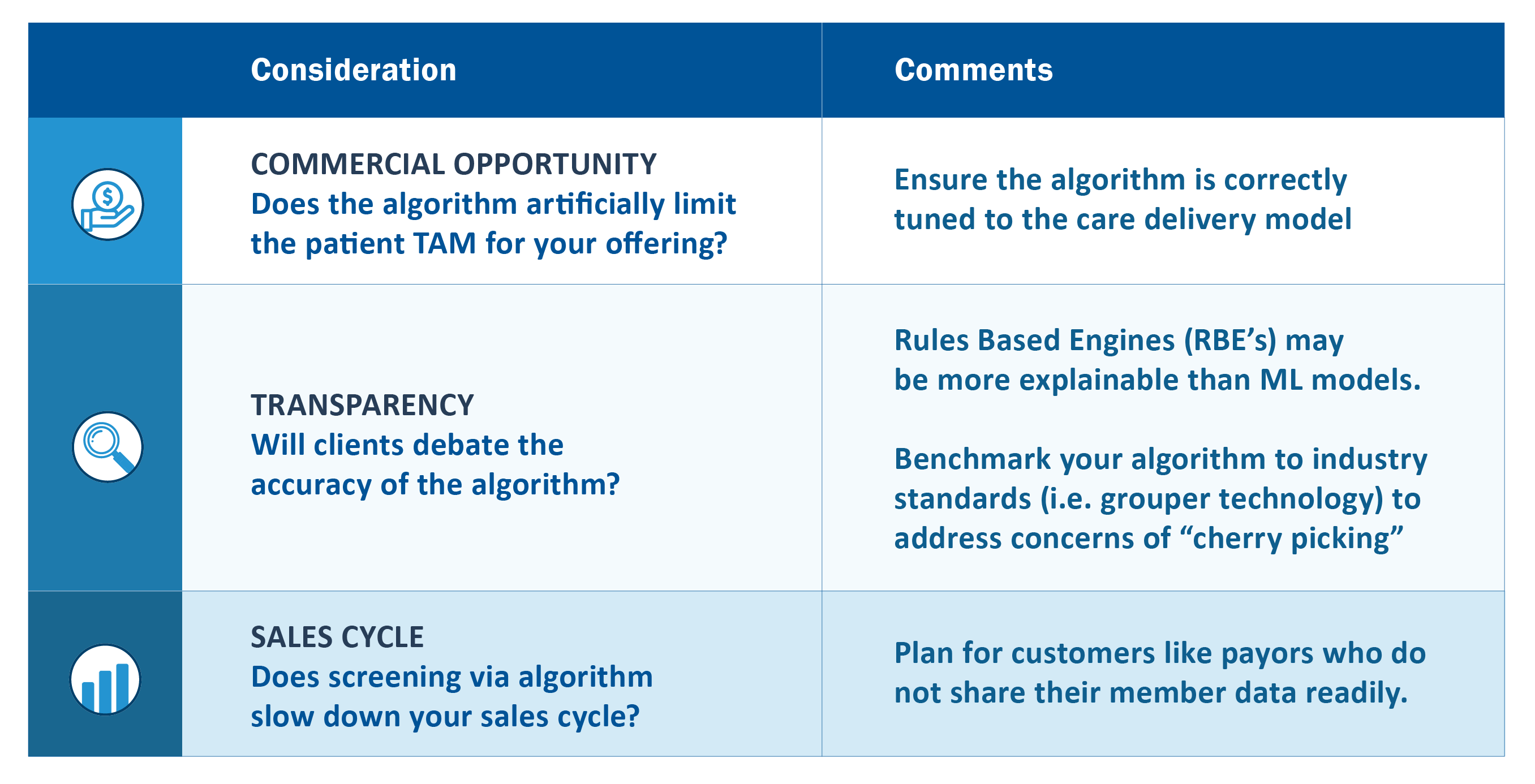
Imagine leaders also observed the importance of aligning AI tools with commercial opportunity, company values like transparency, and sales cycles:
Algorithmically-Driven Patient ID Tools require some foresight on key questions
Releasing a new AI/ML model
The real opportunity here isn’t just about adopting AI—it’s about shaping it. The next frontier for revenue and volume growth in healthcare services depends on developing smarter, more adaptive AI and machine learning models. And that’s where things get interesting.
Within the development community, the question of how to build these algorithms is an ongoing a source of debate, innovation, and, increasingly, competition. As the AI economy scales, healthcare services ventures find themselves at a crossroads: Do they build a model from scratch? Do they adapt an existing one? Do they leverage the power of open-source tools or align themselves with the big players defining the AI landscape?
For large healthcare organizations, the answer seems obvious—they have in-house IT teams experimenting with custom wrappers around foundational models, fine-tuning algorithms to fit their needs. We have run across all of the major foundational models wrapped in healthcare with Grok being the exception (and more of an emerging player). For smaller ventures, the challenge isn’t just about developing AI; it’s about finding a way to do so efficiently, affordably, and at scale.
Many Options: Companies can adapt their AI/ML solution direction to match their internal level of expertise
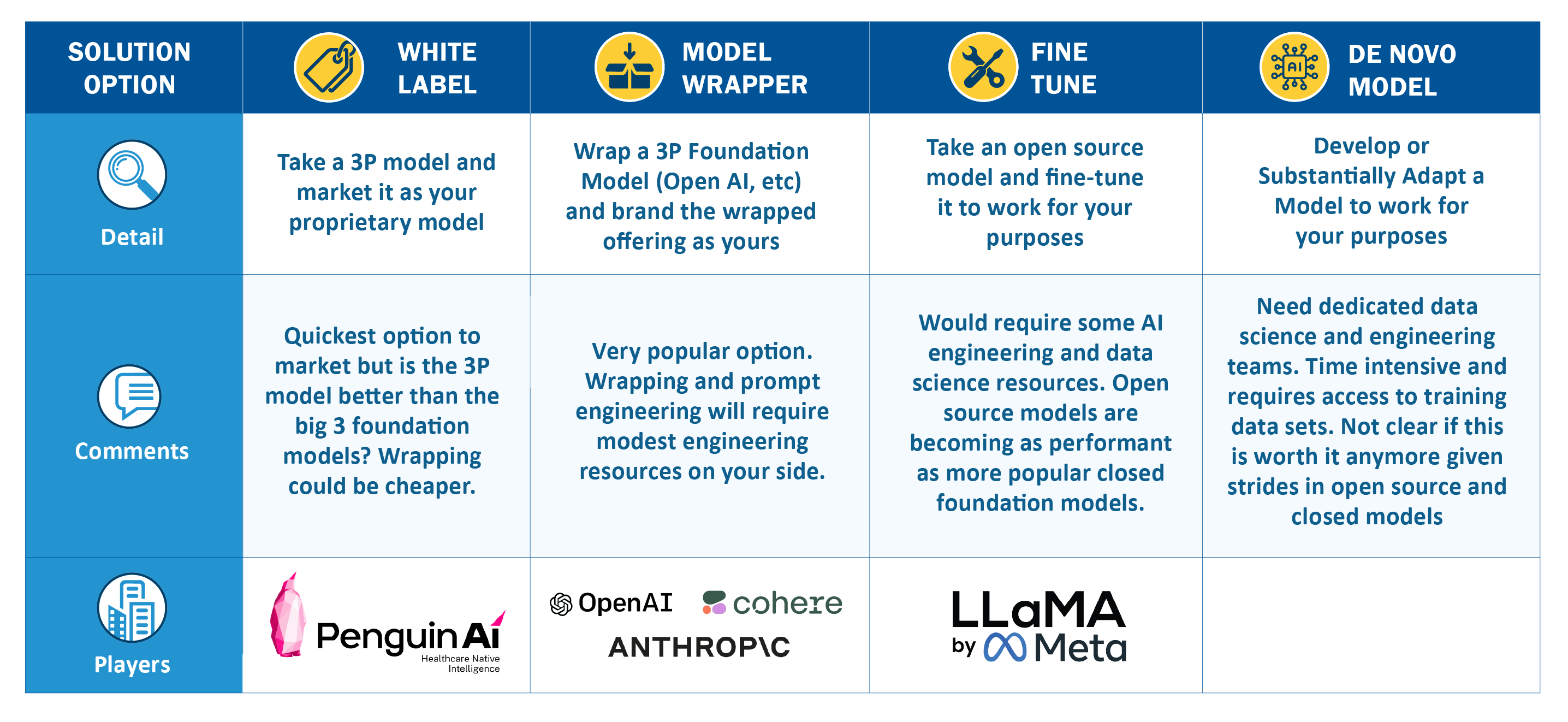
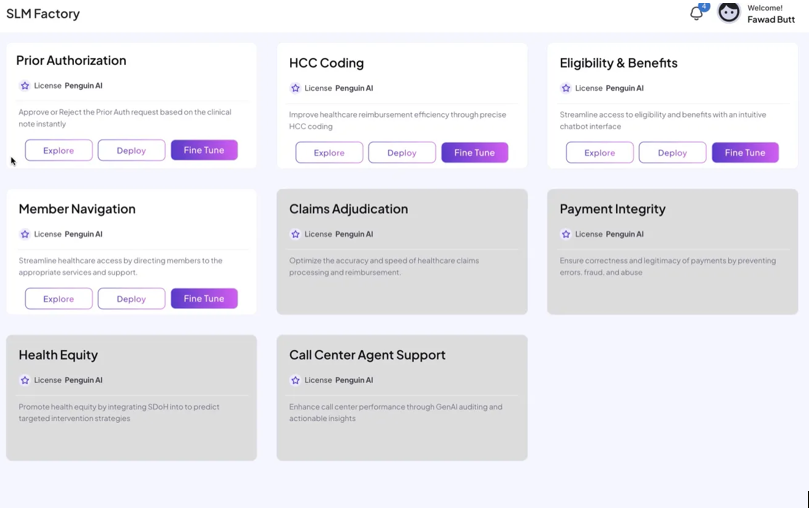
Penguin Ai offers a set of pre-built small language models that can be white labelled for a variety of use cases. The Company’s leadership has a background in the healthcare data space across payors, providers and revenue cycle management.
Penguin has emerged as a key member of several workgroups in the Coalition for Health AI (CHAI), which is a collaborative initiative aimed at promoting the responsible development and deployment of artificial intelligence in healthcare. It brings together leaders from academia, industry, government, and healthcare organizations to establish best practices, standards, and guidelines that ensure AI in health is safe, effective, equitable, and transparent.
A speedy option when AI is a key capability, Penguin now offers the CHAI “nutrition facts” labels for each of their models to help drive transparency in their model development methodology.
“As a former buyer, I spent hundreds of millions customizing generic platforms for healthcare. With Gen AI, we can achieve previously impossible outcomes, leveraging our deep understanding of the healthcare ecosystem to solve its most cumbersome problems. A lot of healthcare companies need AI models but don’t have the internal expertise to wrap or fine tune models. Penguin offers those players a rapid option to deploy and rebrand a portfolio of small models made for specific healthcare use cases.”, says Fawad Butt, Founder &CEO, Penguin Ai and former Chief Data Officer, Kaiser Permanente, United Healthcare & Optum.
The Penguin Offering: Off the shelf small-language models for deployment
Ambient Scribing
Not long ago, Ambient Scribing was heralded as a breakthrough—a technology poised to free physicians from the tyranny of their keyboards, restoring their focus to the patient rather than the screen. The headlines were breathless, the demos impressive, the promise seductive: AI-powered scribes would silently document patient encounters, lifting the administrative burden that has long been the scourge of modern medicine.
Within Rubicon’s portfolio, the peak of this hype cycle already feels like a distant memory. A year ago, interest was at its zenith. Now, after rounds of demos and trials, many of our physicians have seen these tools in action. And what’s become clear is that the market is now flooded with new entrants—each promising a more seamless, more intuitive, more game-changing experience.
This influx serves as a stark reminder of a fundamental truth in AI: true product moats are rare. In a field where innovation moves at breakneck speed, differentiation is fleeting, and yesterday’s disruptor is today’s commodity.
Two dominant categories of players are beginning to emerge. Standalone AI agents—independent, vendor-agnostic tools designed to integrate across multiple systems—are vying for position against EMR-native solutions, those built directly into electronic medical record platforms. The distinction between these two camps is far from rigid, with some solutions blurring the lines.
The question now is whether any of these players can rise above the fray—not just by delivering a technically impressive solution, but by embedding themselves so deeply into the physician’s workflow that they become indispensable. Because in AI, as in medicine itself, the difference between novelty and necessity makes all the difference.
Ambient Scribing Product Categories: EMR players are a recent entrant
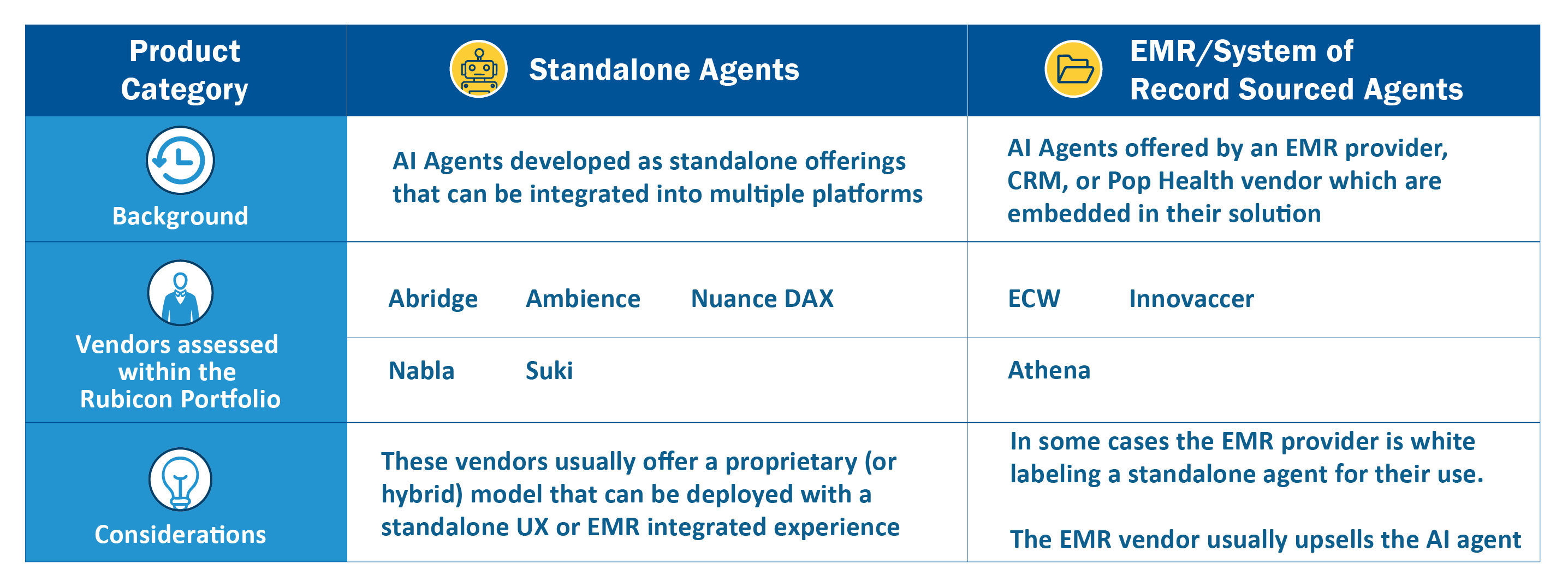
“Ambient Scribes are on the verge of being ready for a physician specialist and we get a high level of interest in these solutions from the Evergreen affiliated nephrologists. Some of the scribes struggle with specialty terminology and workflow. One vendor we demo’ed didn’t pick up a Chronic Kidney Disease related issue in a conversation. But we do see the technology advancing and improving in this area,” says Tim Pflederer, Chief Medical Officer at Evergreen Nephrology.
The scribe offerings appear to be converging around a generally acceptable and usable product – it’s unclear if one platform has achieved true differentiation in the market. If one company has an edge, Ambience AI appears to have created a distinct offering, emphasizing their model’s capacity for edge cases.
HarmonyCares went through a recent Ambience evaluation. Their risk-based documentation suggestions are strong compared to the competitors. They offer good detailed prompting on additions to the note. Most of this technology does well in the typical 4-wall physician office and we are now trying to evaluate how this technology would do in our home visit setting,” says Jeffrey Stevens, Chief Medical Information Officer at HarmonyCares.
“When exploring scribing solutions, we need to take into account the unique needs and nuances of pediatric populations and ensure that the model incorporates accurate measures and information that is specific to our model and the children we serve,” says Eden Klein, Chief Technology Officer at Imagine Pediatrics.
“We are getting strong adoption across specialties and subspecialties within health systems. And ambient scribing is just part of the value we are delivering. We are serving customer needs in care coordination and revenue cycle today,” says Michael Ng, Co-Founder and CEO at Ambience.
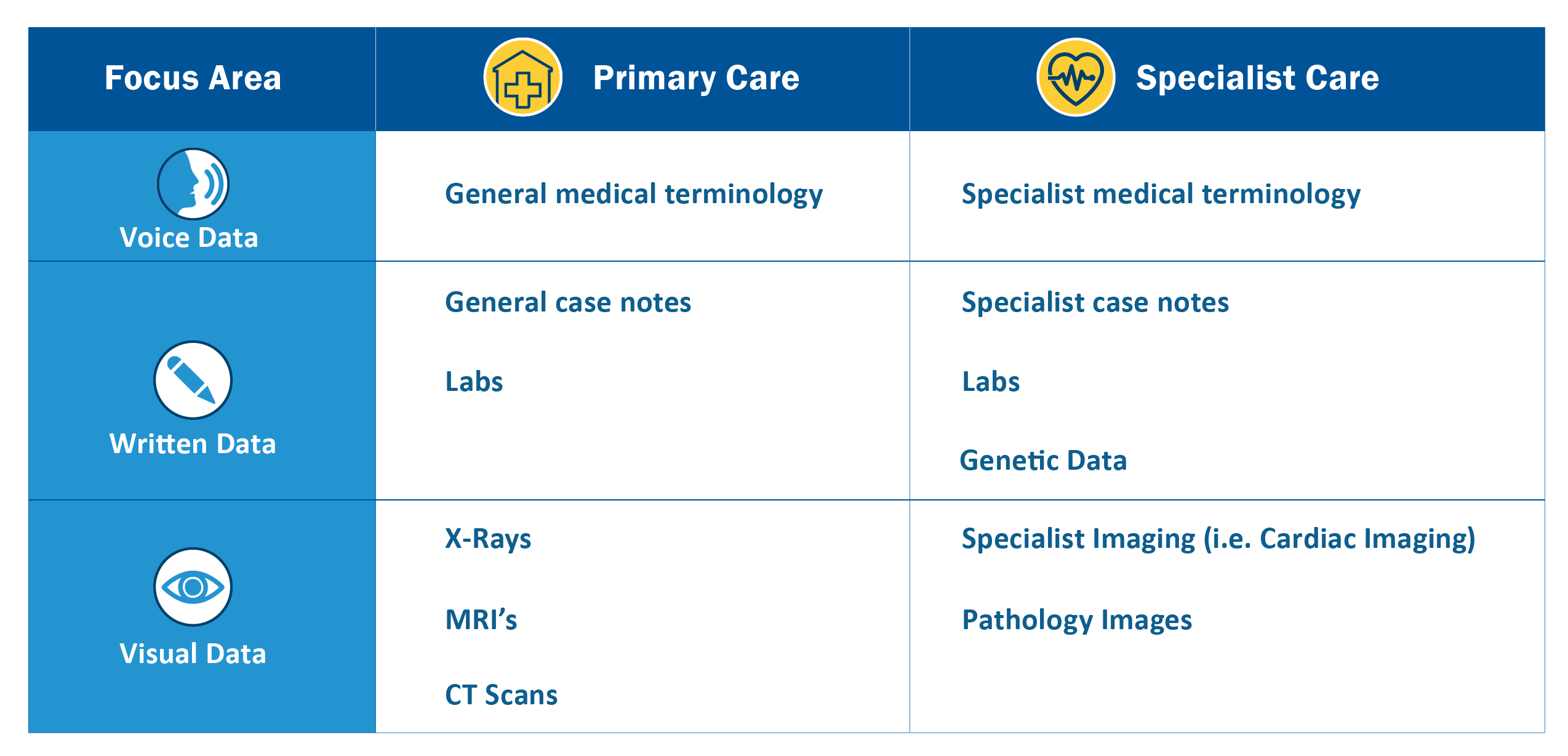
Across conversations with AI vendors — one issue keeps surfacing: training set limitations.
Some vendors hesitate to deploy their models in specialist settings, citing concerns that their training data skews too heavily toward primary care. Others, by contrast, insist their models are robust enough to serve both primary care physicians (PCPs) and specialists, despite clear differences in the way these two groups document and interpret medical data.
At the heart of the debate is a fundamental question: Are AI models truly universal, or do their training sets inherently restrict their capabilities?
On paper, many vendors claim their models can seamlessly transition between PCPs and specialists. But in practice, the underlying datasets tell a different story—one where a model trained predominantly on generalist encounters may struggle with the nuanced language, diagnostic complexity, and workflow idiosyncrasies of specialty care.
The tension speaks to a larger reality in AI-driven healthcare: a model is only as good as the data that shaped it. And until vendors acknowledge the limits of their training sets, the promise of a one-size-fits-all AI solution may remain just that—a promise, rather than a reality.
Training Data: The difference between Specialists and Generalists may have an impact
The entrance of EMR vendors into this space as another interesting development, with Athena taking a notably distinctive approach: allowing users to pick an ambient scribe from 3 different vendor options (including Suki and Abridge).
US Heart & Vascular “USHV,” a Rubicon portfolio company and cardiology physician practice management platform, is an eCW user and has been evaluating their new scribe Sunoh.
“We opted to implement eClinicalWorks (eCW) as our unified EHR platform and for us its essential that AI-driven tools are deeply embedded within the EHR. eCW has taken a unique approach - investing in and developing these capabilities in-house with their Sunoh.ai ambient listening scribe. We are also excited to deploy their healow Genie AI-powered patient engagement platform,” said Irfan Ali, Chief Information Officer at USHV.
“We offer Suki Assistant, a full featured AI assistant that handles a wide breadth of tasks from documentation to coding to patient summaries for health systems and clinics looking to help their clinicians save time; we also offer our AI engine, Suki Platform, to technology companies looking to add AI experiences to their solutions. We’re proud to partner with EHRs, including Athena, telehealth organizations like Zoom, clinician communications companies, and more to power their AI experiences,” says Punit Singh Soni, Founder and CEO at Suki.
Use cases in specialties and care management are driving continued feature development in Ambient Scribing, for example:
- Specialist Care Orders: If the Ambient Scribe could generate orders for a specialist based off a conversational situation that would be a huge unlock.
“When vendors can automate the generation of orders in the EMR that will be an order of magnitude improvement in terms of time saved by the specialist physician. You can do the work of a visit in the course of a conversation,” says Tim Pflederer, Chief Medical Officer at Evergreen Nephrology.
- Care Management: Ambient scribes have been focused on physicians, but in value-based care settings, the care manager becomes an integral part of care delivery infrastructure. In response, companies like Innovaccer are developing an ambient scribe for care managers.
“AI in healthcare isn’t just about efficiency; it’s about ensuring every interaction between care teams and patients translates into better health outcomes. InScribe for care managers is designed to do just that—bridging technology with compassion to meet the unique needs of value-based care. This is just the beginning. As we expand our AI capabilities, we’re introducing a suite of new copilots and intelligent agents tailored for care management, risk stratification, and quality improvement,” says Sandeep Gupta, Co-Founder and COO at Innovaccer.
Risk Stratification
In the shifting landscape of value-based care, one tool has emerged as essential: risk stratification models. These algorithms are becoming the backbone of modern care organizations, transforming healthcare from a reactive, fee-for-service treadmill into a proactive system that identifies and manages high-risk patients before they spiral into costly medical crises.
From a financial perspective, the stakes couldn’t be higher. A well-calibrated risk model, when paired with next-best-action clinical interventions, has the potential to bend the cost curve, reducing unnecessary hospitalizations and lowering overall medical spend. But the real question is: can AI push these models beyond their traditional limitations? Can it predict severity and future spend with a level of precision that old, rules-based systems never could?
One emerging player betting big on that premise is Delorean AI—a company that has drawn interest from multiple Rubicon portfolio ventures. Their approach blends rules-based engines with black-box AI models, a hybrid strategy designed to extract deeper insights from complex patient data.
What sets Delorean apart is the scale of its training ground. Their models were honed on a massive dataset of 40 million claims from UnitedHealthcare, and the company isn’t shy about making bold claims: 80-90% predictive accuracy compared to 60% from legacy Optum models.
Delorean’s strategy isn’t just about broad predictive power—it’s targeted. They offer off-the-shelf risk stratification models focused on high-impact disease states: renal, diabetes, cardiovascular, mental health, and respiratory conditions. The goal? To move beyond static risk scores and into real-time, AI-driven forecasting—an intelligence layer that could revolutionize how healthcare systems anticipate and prevent deterioration.
But as with any black-box AI model, the question remains: can it be trusted? Accuracy claims are one thing—proving real-world impact is another. If successful in proving out the model, Delorean is positioned to set the pace in this important segment.
“Our Real-Time and Future Risk Stratification is a first in the healthcare industry. It can not only assess a patient’s risk in real time but also predict future risks—what is the delta and how to reduce these scores. We are essentially the Future for Healthcare,” says Severance MacLaughlin, CEO and Co-Founder, Delorean AI.
The Delorean Interface flags patients in need of likely interventions to get ahead of MLR expenditures
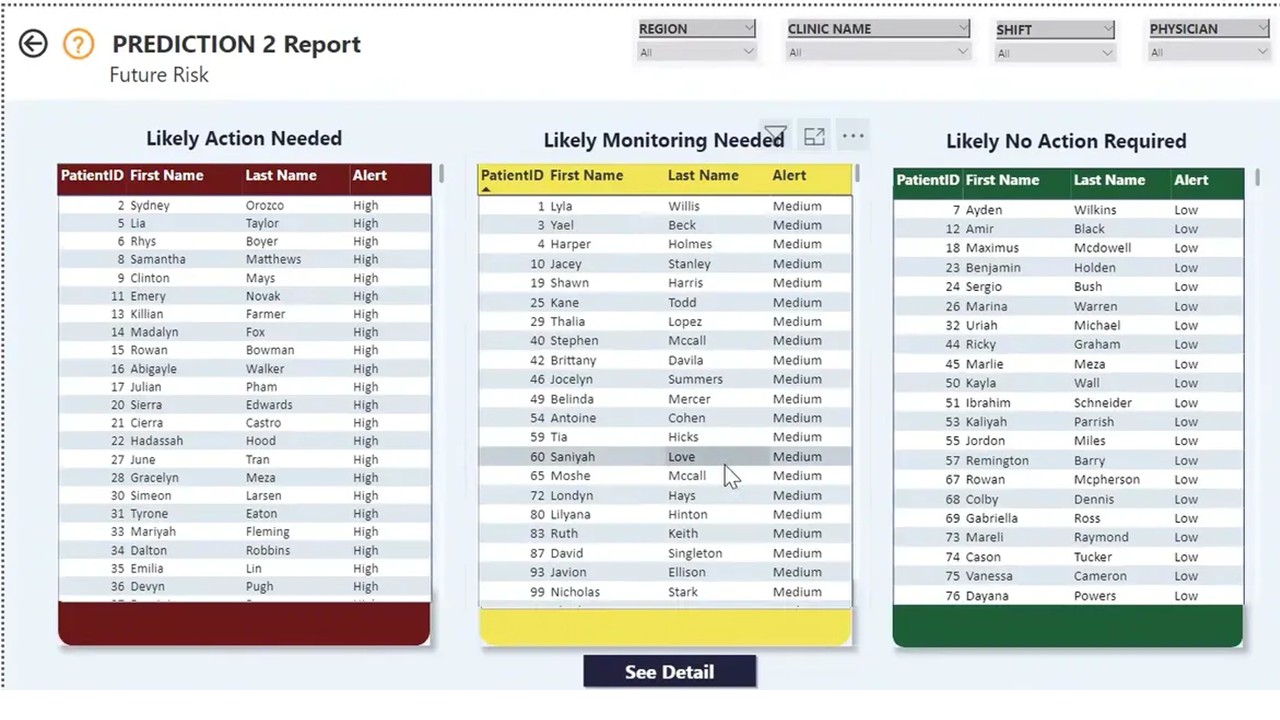
Note from Delorean AI: The content used in the slide above is synthetic data
“The use of AI for risk stratification in the renal use case is promising but we still need to see additional improvement before this tech is deployment ready,” said Ron Margalit, Chief Information Officer at Evergreen Nephrology.
In the delicate world of hospice care, timing is everything. The ability to anticipate a patient’s decline—not just in broad clinical terms, but with granular, data-driven precision—can mean the difference between a well-managed, dignified transition and a crisis that leaves families and caregivers scrambling.
Medalogix Muse, an AI-powered platform, is quietly reshaping how hospice providers assess patient risk. Unlike traditional models that rely on structured medical data, Muse taps into unstructured EMR data, extracting signals from clinician notes, assessments, and patient histories to calculate risk scores for transition risk, mortality risk, and overall patient risk.
What sets Medalogix apart is its deep integration with Homecare Homebase (HCHB)—the dominant EMR system in the hospice sector. This tight coupling allows the platform to seamlessly ingest raw, unstructured data, pass it through natural language processing (NLP) and machine learning algorithms, and surface actionable insights for hospice teams.
The result? A population health dashboard that lets providers sort and stratify patients by risk level, helping them prioritize care for those most in need. In an industry where staffing shortages and unpredictable disease trajectories make resource allocation a constant challenge, having an AI-driven roadmap for patient decline is a powerful proposition.
Medalogix claims substantial penetration within the HCHB user base, a sign that hospice providers are increasingly willing to lean on AI in what is, arguably, one of the most sensitive and human-centered branches of medicine. But the real test lies ahead: can AI-driven risk stratification truly improve end-of-life care, or will it become just another layer of prediction in a field that ultimately defies perfect foresight?
The Muse Interface offers individual and population-level views of patient risk in the Hospice setting.
Muse offers an individual deep dive on predictive metrics in a hospice setting
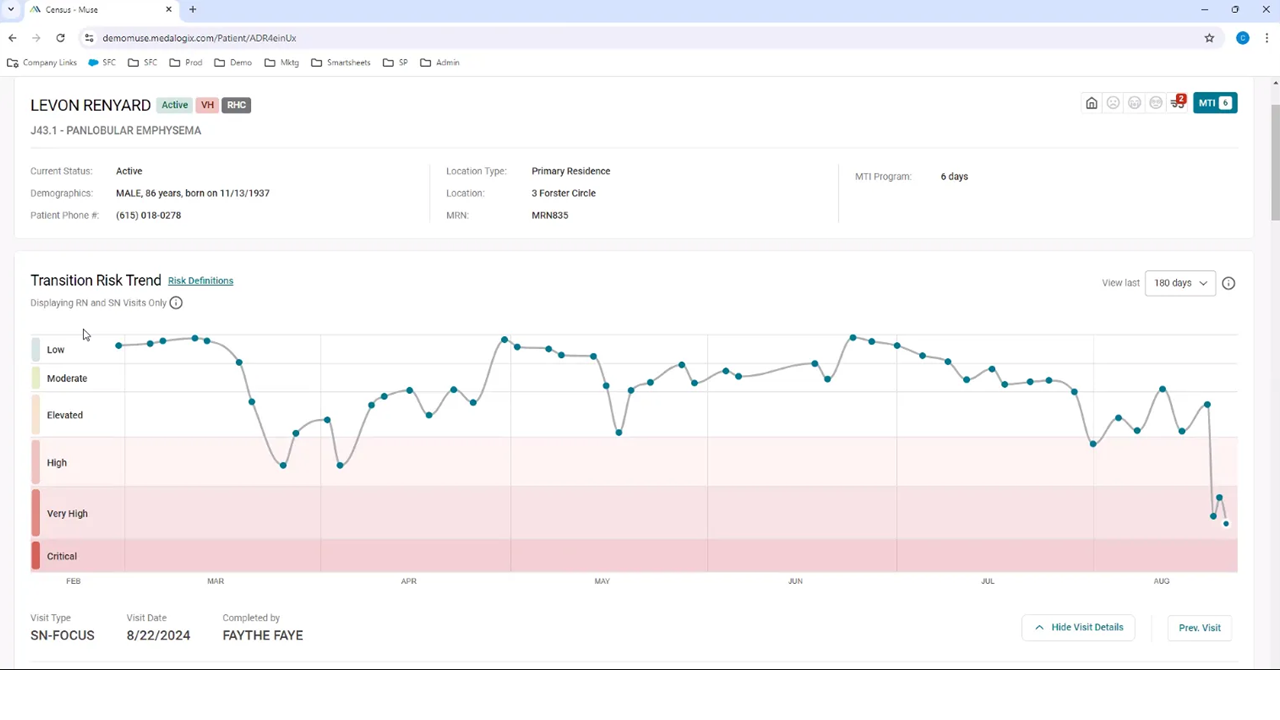
Muse also offers a more aggregated view of the patient panel
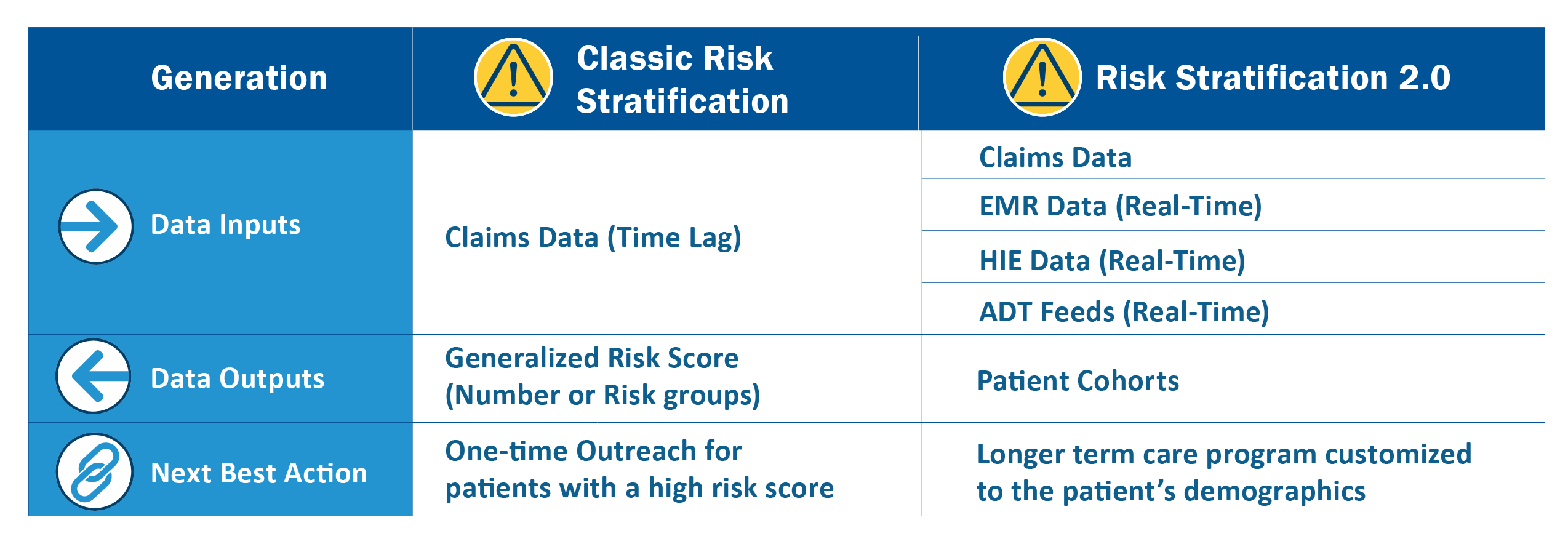
For Imagine Pediatrics, a company dedicated to caring for children with complex medical and behavioral health needs, the traditional and emerging risk stratification models simply weren’t enough. They needed something faster, smarter, and more precise—a system that could move beyond the lagging indicators of the past and provide real-time, actionable insights for a population where every moment counts.
In most of the industry, risk stratification has long been claims-driven. It’s a familiar approach—using insurance claims data to assess patient risk—but it comes with a fatal flaw: time lag. Claims data can be weeks or even months old, leaving providers reacting to problems instead of anticipating them. Instead of relying solely on claims, Imagine built a model that integrates real-time data from multiple sources: their EMR, Health Information Exchanges (HIEs), additional rich data streams, and their own proprietary insights. This multilayered approach allows them to capture a more dynamic and accurate picture of patient risk, giving providers early warning signals rather than delayed snapshots.
But the potential breakthrough is in how this data is applied. Most risk models distill patients down to a single score—a number that signals risk level but offers little in terms of tailored care. Imagine Pediatrics has taken a different approach. Instead of assigning a static risk score, they segment patients into cohorts based on a highly individualized model of medical and behavioral pathways.
These cohorts are actionable, meaning they’re directly linked to specific interventions, personalized treatment plans, and targeted care journeys. For children with special health care needs, this level of precision isn’t just useful—it’s game-changing. It allows for more timely, more effective, and more personalized interventions, ensuring that the right resources reach the right patients at the right time.
“Our unique approach to risk stratification and the leveraging of real time data is a game changer for us because our patients have unique, individualized needs and are quite vulnerable at discrete times, including the moment of discharge from an acute setting. The combination of rich data sets and input from our multidisciplinary, pediatrician-led clinical team, enables us to generate insights on the right type of care each patient needs at any point in time and drives clinical teams to next best actions,” said Eden Klein, CTO at Imagine Pediatrics.
The Imagine Pediatrics Model: To go beyond simple risk stratification to actionable patient cohorts
Despite some success in this area, many healthcare leaders continue to voice skepticism based on historical experiences with risk stratification models:
“There continues to be a paucity of risk stratification algorithms that can actually drive the care team to a good next best action. It makes me wonder if the risk stratification algorithmic market is a commodity market with little differentiation. It has to turn into work that matters,” said Bartley Bryt, Chief Medical Officer at Privia Health.
“Part of the problem is the experience specialists have had to date with more immature models. Risk Stratification algorithms that serve up specific diagnostic code recommendations on patients can quickly lose credibility if those codes are a total mismatch with the patient type (i.e. diabetic codes for a non-diabetic),” says Pflederer, Chief Medical Officer, Evergreen Nephrology.
Overall, we see a need for a new generation of risk stratification - “Risk Stratification 2.0” - that uses an approach like the one deployed by Imagine Pediatrics to address some of these concerns.
Technology could help make Risk Stratification more actionable
Parting Thoughts

AI is often framed as a clinical revolution, a toolset that will transform diagnostics, treatment plans, and patient engagement. But beneath that lofty promise lies an equally compelling, if less glamorous, reality: AI’s potential to reshape the financial picture of healthcare services.
Early financial models suggest modest AI-driven efficiencies can unlock significant EBITDA growth. And that financial health—often overlooked in conversations about AI—directly translates to mission sustainability. A more profitable healthcare organization is one that can invest more in patient care, expand services, and improve outcomes.
Across our portfolio, AI innovation is in full swing. Categories like Ambient Scribing and Risk Stratification are seeing rapid adoption, though some markets—especially Ambient Scribing—are becoming crowded.
Yet, not every healthcare AI use case lends itself to black-box machine learning models. In domains where explainability and transparency matter, rules-based engines still have a role to play—and they are unlikely to vanish. Algorithmic identifier-driven business models serve as a prime example: where precision matters, buyers are reluctant to trust opaque AI outputs without human oversight. That’s why many organizations are deploying human-in-the-loop AI, a strategy that balances automation with clinician judgment. Looking ahead, we’ll continue to explore the evolving landscape of AI in healthcare, with a focus on:
- Population health software and insights from Rubicon companies working with vendors like Zus and Innovaccer.
- The rise of back-office automation tools like Tennr and voice AI agents like Hippocratic AI—and how agentic AI models could redefine efficiency in healthcare.
The AI revolution in healthcare is far from settled. The question isn’t whether AI will reshape the industry—it’s which models, which approaches, and which business strategies will prove most enduring, and we look forward to exploring it all with you here.
Individuals Interviewed for this Article
Rubicon Portfolio Companies
 Jason Foucher, Chief Product Officer, Indigo
Jason Foucher, Chief Product Officer, Indigo Eden Klein, Chief Technology Officer, Imagine Pediatrics
Eden Klein, Chief Technology Officer, Imagine Pediatrics Meghan Haycraft, Co-Founder & Chief Strategy Officer, Imagine Pediatrics
Meghan Haycraft, Co-Founder & Chief Strategy Officer, Imagine Pediatrics Sonnie Linebarger, CEO, Cadre Hospice
Sonnie Linebarger, CEO, Cadre Hospice Ron Margalit, Chief Information Officer, Evergreen Nephrology
Ron Margalit, Chief Information Officer, Evergreen Nephrology Tim Pflederer, Chief Medical Officer, Evergreen Nephrology
Tim Pflederer, Chief Medical Officer, Evergreen Nephrology Joe Lucero, Vice President of Risk Adjustment, Honest Health
Joe Lucero, Vice President of Risk Adjustment, Honest Health Jeffrey Stevens, Chief Medical Information Officer, HarmonyCares
Jeffrey Stevens, Chief Medical Information Officer, HarmonyCares Bartley Bryt, Chief Medical Officer, Privia Health
Bartley Bryt, Chief Medical Officer, Privia Health Irfan Ali, Chief Information Officer, US Heart and Vascular
Irfan Ali, Chief Information Officer, US Heart and Vascular
AI Technology Vendors
 Fawad Butt, CEO, Penguin Ai
Fawad Butt, CEO, Penguin Ai Ronen Lavi, CEO, Navina
Ronen Lavi, CEO, Navina Jay Ackerman, CEO, Reveleer
Jay Ackerman, CEO, Reveleer Michael Ng, Co-Founder and CEO, Ambience Healthcare
Michael Ng, Co-Founder and CEO, Ambience Healthcare Sandeep Gupta, Co-Founder and COO, Innovaccer
Sandeep Gupta, Co-Founder and COO, Innovaccer Severence MacLaughlin, CEO and Co-Founder, Delorean AI
Severence MacLaughlin, CEO and Co-Founder, Delorean AI Punit Singh Soni, Founder and CEO, Suki
Punit Singh Soni, Founder and CEO, Suki





